- View Course & Enroll

Dialogue in Therapy: The Art of Presence
FRIDAY, JUNE 21 – SUNDAY, JUNE 23, 2024
10:00 AM – 5:00 PM EST. with lunch and 2 breaks.
ONLINE/HYBRID: Join me on Zoom or attend at Yale University, New Haven, CT.A three-day introduction that focuses on the relational skills to foster new possibilities of hope. CEUS
- View Workshop & Enroll

Open Dialogue Skills for Parents of Teenagers and Young Adults
NEW PARENTING WORKSHOP ADDRESSING THE YOUTH MENTAL HEALTH CRISIS — For parents of children dealing with mental health problems. This 8-week, 2-hour weekly online workshop series teaches the core skills of healing communication. Next dates: TBA
- Read More
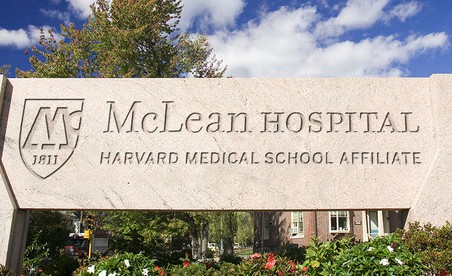
McLean adopts Dialogic Practice
See the new Harvard/McLean research study that reports positive results.



